Abstract
Introduction:
Cytogenetic features at diagnosis have significant independent prognostic impact in acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL). Failed or unsuccessful cytogenetics (UC) is estimated to occur in 10% of AML cases and 25-30% of ALL cases (Grimwade, 2010; Pullarkat, 2008). Previous studies suggest worse outcomes in AML patients (pts) with UC, similar to pts with unfavorable karyotype with lower response rates to induction chemotherapy and poor 5-year (yr) survival rates (Medeiros, 2014; Lazarevic, 2015). Hydroxyurea (HU) and steroids are often given urgently for cytoreduction prior to obtaining cytogenetics. The effects of such pretreatment on rates of UC have not been studied previously. In this study, we compared clinical outcomes of acute leukemia pts with UC versus successful cytogenetics (SC) and determined whether the use of HU or steroids affects cytogenetics success rates.
Methods:
All pts <70 yrs with de novo acute leukemia (AML or ALL) with available diagnostic bone marrow and cytogenetics testing seen at the Leukemia/Bone Marrow Transplant (BMT) Program of British Columbia between January 2010 and December 2016 were included. Pertinent information was reviewed from the program database. Cytogenetic failure was defined by the presence of <10 metaphases with a normal karyotype in the absence of a clinically actionable FISH abnormality. Pts with SC were risk stratified based on NCCN guideline criteria (NCCN, 2018). Baseline features of pts with SC and UC were compared using Chi-squared and two-tailed t-testing. Overall survival (OS) was calculated from the date of initial diagnosis to the date of death from any cause. Disease free survival (DFS) was calculated from the date of attaining first complete remission (CR1) to the date of relapse or death from any cause. Survival outcomes were estimated using the Kaplan-Meier method, with p values determined using the log rank test. A p < 0.05 was considered significant.
Results:
We identified 654 cases of acute leukemia (AML N=515; ALL N=139). Of these, 39 (6%) had UC (AML N=16, 3%; ALL N=23, 17%). There was no difference in age at diagnosis between groups (UC vs SC, 46 vs 51 yrs, p=0.08). AML pts with UC had higher initial white blood count (WBC) at diagnosis (71 vs 34, p<0.001). No effect of WBC was seen in ALL pts with UC versus SC. HU and/or steroid use prior to cytogenetics was similar between UC and SC groups in both AML and ALL pts (UC vs SC, HU: 8% vs 12%, p=0.61; steroids: 5% vs 1%, p=0.07. Therapy with intensive induction was also similar between groups (UC vs SC, 92% vs 90%; p=1.00). 137 (27%) of AML pts with SC had favorable risk disease, 182 (37%) intermediate, and 180 (36%) high risk. In ALL pts with SC, 32 (28%) had standard risk, and 84 (72%) had high risk disease. Follow up time in UC and SC groups was similar (32 vs 27m, p=0.18).
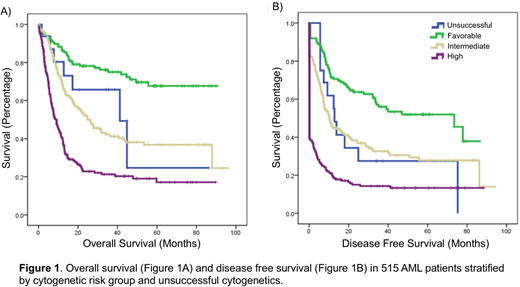
CR rates in AML pts with UC was 81%, which was similar to pts with intermediate risk disease (84%, p=0.72) and better than CR rates of 39% observed in high risk pts (p=0.03). Compared to pts with SC, AML pts with UC had similar 5-yr OS and DFS as pts with intermediate risk disease (5-yr OS 25% vs 37%, p=0.45; 5-yr DFS 28% vs 28%, p=0.84), superior survival to high risk pts (5-yr OS 25% vs 17%, p=0.01; 5-yr DFS 28% vs 13%, p=0.036), and inferior survival to favorable risk pts (5-yr OS 25% vs 68%, p=0.07, 5-yr DFS 28% vs 52%, p=0.008), Figure 1.
CR rates in ALL pts with UC was 83% and not significantly different than standard (94%, p=0.22) or high risk pts (86%, p=0.74). Compared to pts with SC, ALL pts with UC had similar 5-yr OS and DFS to pts with standard and high risk disease (UC vs standard vs high; 5-yr OS 58% vs 51% (p=0.93) vs 55% (p=0.85); 5-yr DFS 50% vs 37% (p=0.86) vs 36% (p=0.27)). Subgroup analysis of UC pts demonstrated no difference in survival in UC pts receiving BMT (N=12) vs no BMT (N=27). UC pts with high WBC >20 (N=14) had inferior survival compared to those with WBC ≤ 20 (N=25) (5-yr OS 60% vs 29%, p=0.025; 5-yr DFS 52% vs 12%, p=0.013).
Conclusions:
Unsuccessful cytogenetics was more frequently observed in ALL as compared to AML pts, though at lower rates than reported in previous studies. HU and steroid use had no effect on the rates of cytogenetic success. In comparison to previous reports, UC in AML was not associated with inferior outcomes, and survival was similar to intermediate risk pts. High initial WBC count was prognostic in pts with UC, and further studies are warranted to evaluate factors that affect outcomes in pts with UC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal